Anais Lemoine, a paediatrician at APHP’s Trousseau hospital, did her PhD at Micalis, in the Probihôte team. This study is the result of collaboration with clinicians from the APHP at Trousseau and Pitié-Salpétrière hospitals and two INRAE laboratories at UPSaclay (Micalis and MTS/LIAA).
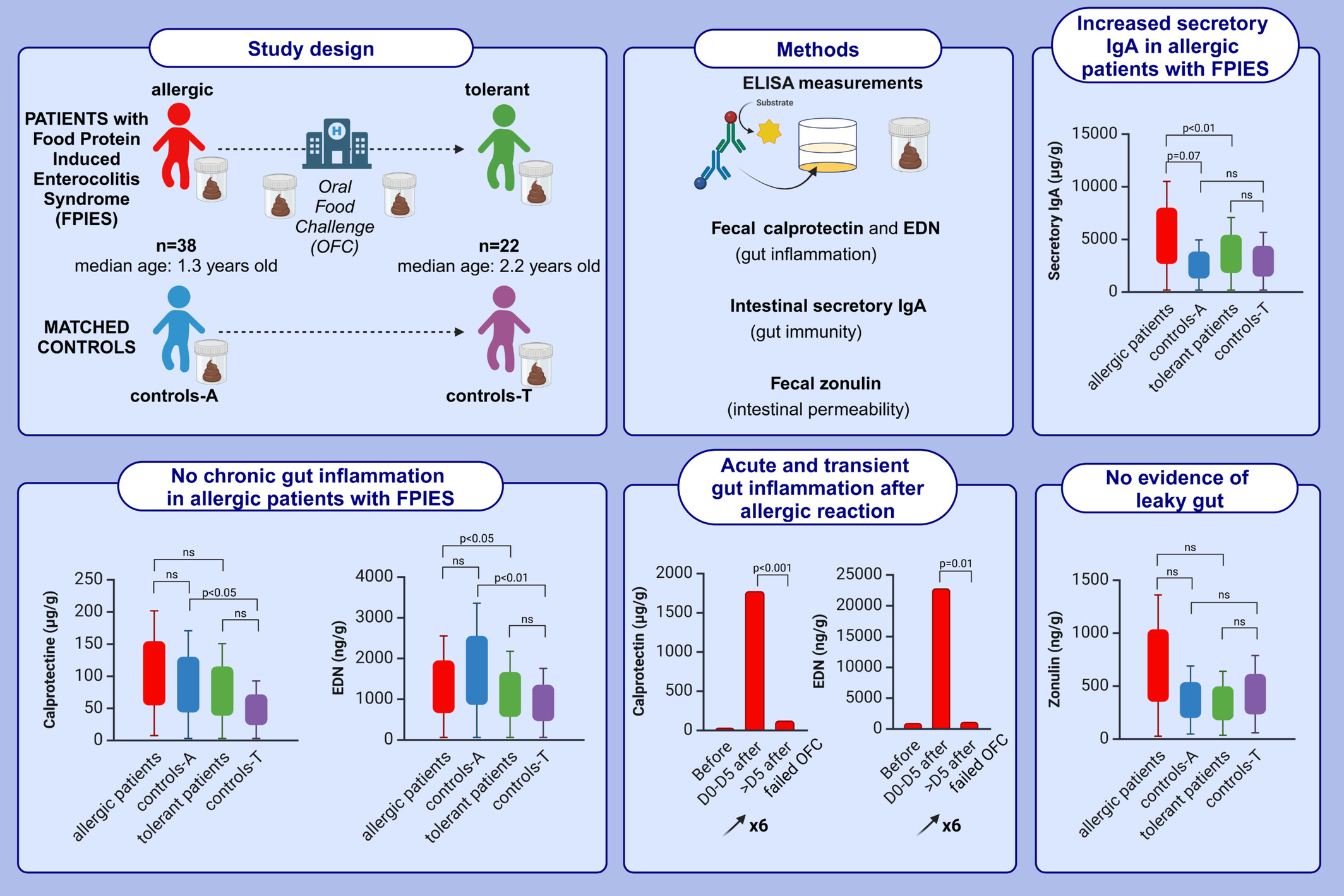
Food protein-induced enterocolitis syndrome (FPIES) is a non-IgE-mediated allergy without known biomarkers. We aimed to compare fecal biomarkers related to gut inflammation and immunity in children with FPIES, with resolved FPIES (tolerant), and in matched controls. As with other food allergies, consumption of the culprit food (mainly cow’s milk) causes allergic symptoms, but FPIES symptoms tend to be digestive and neurovagal (e.g. profuse vomiting, lethargy and paleness).This study is the first case–control cohort of children with FPIES with a longitudinal follow-up until tolerance acquisition.
We evidenced that:
- Allergic patients with FPIES under exclusion diet of the culprit food had no measurable gut
inflammation (fecal calprotectin and EDN). - Allergic patients had chronic increased fecal secretory IgA concentrations compared to controls
and even to tolerant patients. - After exposure to the culprit food inducing clinical symptoms, we observed significant
transitory increase of f-calprotectin and f-EDN concentrations, indicating an acute gut
inflammation, which then returned to normal values within one week. - Zonulin was stable in patients during follow-up, and comparable to controls.
We propose secretory IgA as an interesting predictive biomarker for clinicians and patients for predicting allergy remission.
This work is being pursued through the study of faecal and salivary microbiota and large-scale metabolites.
Contact:
Links:
https://onlinelibrary.wiley.com/doi/10.1111/all.16457